Postpartum Depression among Adolescent Mothers in the United States
Photo by Sarah Chai from Pexels
By Susan May
Published Spring 2022
Special thanks to Jamie LeSueur for editing and research contributions
Summary+
Adolescent mothers are twice as likely to suffer from postpartum depression than adult mothers. In addition, teen moms are more likely to experience social stigma associated with teenage pregnancy and motherhood. Adolescent mothers also abuse substances at a higher rate than adult mothers, and teen dads are less likely to be involved in parenting responsibilities than adult fathers. These factors associated with teenage mothers cause an increased likelihood of teen moms developing postpartum depression. When mothers suffer from postpartum depression, their children are more at risk for child development problems, fathers are more likely to suffer from depression, and parents are less likely to run an efficient household. Additionally, severe postpartum depression or psychosis greatly increases maternal suicide and infanticide. Successful treatments for postpartum depression include breastfeeding and interpersonal psychotherapy.
Key Takeaways+
- Postpartum depression causes mothers to withdraw from loved ones, feel numb or disconnected from their baby, worry that they will hurt their baby, and feel guilty about not being a good mom.121
- Social stigma against teen moms puts adolescent mothers at a higher risk for developing PPD.
- Teen fathers are less likely to be involved in parenting with their child’s mother, which increases adolescent mothers’ likelihood of developing PPD.
- Child development, specifically academic achievement and behavioral patterns, are negatively affected in children whose mothers suffer from PPD.
- Postpartum psychosis, an escalation of PPD, is associated with higher rates of infanticide and maternal suicide.
- Researchers have found that breastfeeding and interpersonal psychotherapy (IPT) are methods to lower maternal depression, but mothers feeling depressed should seek a professional medical expert to find a treatment that works for them specifically.
Key Terms+
Postpartum depression (PPD)—Postpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2
Postpartum psychosis (PPP)—Postpartum psychosis (PPP) is an escalation of postpartum depression and a serious mental illness that can cause women to have delusions, hallucinations, paranoia, rapid mood swings, etc., associated with their role as mothers.3
Adolescent mother—A woman who gives birth when they are the age of 19 or younger and chooses to parent their child.
Negative birth experience—When mothers feel extreme pain, fear, or stress during childbirth, it can leave the mother with trauma, impairing her ability to bond with her baby. Negative birth experiences can also affect a woman’s willingness to have another baby and is a risk factor for future experiences with mental illness.
Substance Abuse—Substance abuse occurs when a person consumes too much alcohol, drugs, or other illegal/legal substances or misuses those substances. Addiction and substance abuse are not the same conditions, as people who abuse substances can stop their behavior(s).4
Infanticide—The act of killing a child before they reach the age of 1. The child's parent commits most infanticide cases.
Context
Q: Who are adolescent mothers?
A: Adolescent mothers are women who give birth at age 19 or younger and act as the primary guardian for their child(ren). In the United States, approximately 58% of teenagers who get pregnant choose to raise their child(ren).5 The teen birth rate slowly declined between the years 2009–2019, dropping from 39.1 to 16.7 (births for every 1,000 females ages 15–19).6, 7
Q: What are postpartum depression and its symptoms?
A: Postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth due to stressful life events, low social support, pregnancy complications, negative birth experiencesWhen mothers feel extreme pain, fear, or stress during childbirth, it can leave the mother with trauma, impairing her ability to bond with her baby. Negative birth experiences can also affect a woman’s willingness to have another baby and is a risk factor for future experiences with mental illness., etc.8, 9 PPD is often mistaken for the “baby blues,” which is a less severe hormonal change many mothers experience directly after giving birth. The baby blues cause 70–80% of new mothers to experience some sadness or mood swings in the first 2 weeks after delivery.10, 11 PPD lasts longer than the baby blue’s 2-week period and has severe symptoms: withdrawing from loved ones, feeling numb or disconnected from your baby, worrying that you will hurt your baby, and feeling guilty about not being a good mom.12 Some other health symptoms of PPD include fatigue, insomnia, loss of appetite, and restlessness.13
Q: How long does PPD typically last after a mother gives birth?
A: Women are most at risk for developing postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 in the 3 months after childbirth. PPD usually fades away within a year of the postpartum period, but can last up to 3 years in severe cases.14 Women are encouraged to seek professional medical help if their depression symptoms last more than 2 weeks.15
Q: What percent of adolescent mothers experience postpartum depression?
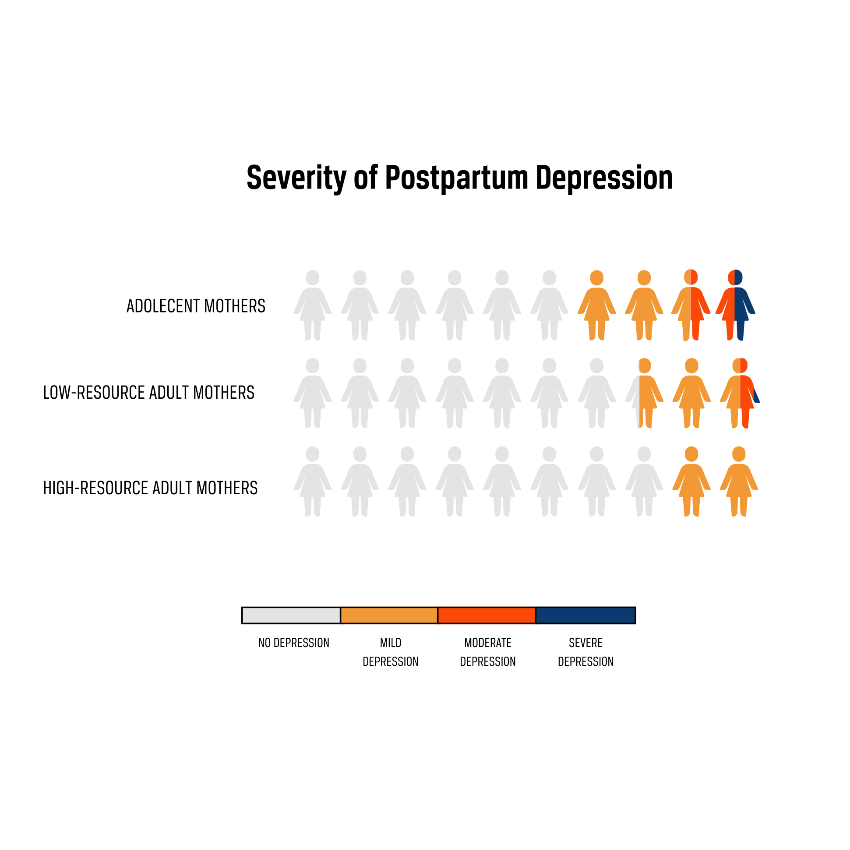
A: An estimated 10–20% of all mothers experience some type of PPD, and this rate is at least twice as high for adolescent mothers.16, 17 One study analyzed the breakdown of depression severity among adolescent mothers at 6 months postpartum and found that 26.9% of adolescent mothers experienced mild depression, 11.3% experienced moderate depression, and 3.8% experienced severe depression.18 These combined results lead to an overall PPD rate of 42%, consistent with the estimate for adolescent mothers. Researchers also evaluated PPD rates in high- and low-resource adults (adults with at least 2 years of college experience and adults with less than 2 years of college experience).19 Teen moms reported higher depressive symptoms in all categories than adults with both high and low resources, so there is evidence that adolescence increases PPD.20
Q: When was postpartum depression first identified?
A: The knowledge that women can experience mental illness and depression after birth has been around since before the common era.21 In the 2nd millennium BCE, all types of depression (including PPD) were called “melancholia” and believed to be a spiritual affliction, not a physical disease.22 Depression was officially tied to the postpartum period in 1994 when the American Psychiatric Association added postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 to the 4th edition of the DSM (Diagnostic and Statistical Manual of Mental Disorders), a book that defines and classifies mental disorders.23 After the medical community officially recognized PPD as a mental illness, increased awareness and improved screening methods caused more women to recognize their symptoms and seek help from medical professionals.24 As a result, the rate of women diagnosed with postpartum depression increased by 30% between 2014–2018.25
Q: How is postpartum depression treated?
A: Medical professionals treat postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 through medication and therapy.26 Some examples of medicine used to manage symptoms of PPD are antipsychotic medications, mood stabilizers, and benzodiazepines.27 The medical community also advises mothers experiencing depression to prioritize self-care, exercise, and participate in meditation therapies like yoga and relaxation training.28
Q: What is postpartum psychosis?
A: Some severe cases of postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 escalate into psychosis, which occurs in less than 0.02% of new mothers.29 Postpartum psychosisPostpartum psychosis (PPP) is an escalation of postpartum depression and a serious mental illness that can cause women to have delusions, hallucinations, paranoia, rapid mood swings, etc., associated with their role as mothers.3 (PPP), while rarer, is a serious mental illness, and its symptoms include delusions, hallucinations, paranoia, and rapid mood swings.30 Additionally, women with PPP are more likely to harm themselves and those around them.31 To treat postpartum psychosis, electroconvulsive therapy (which sends electrical currents through the brain) can be used to change brain chemistry.32
Q: Where is this social issue most prevalent?
A: Rates of postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 are lower in first-world nations and higher in developing countries.33 A study found that in western countries (referring primarily to first-world and high-income nations in Europe and the Americas), the estimated average PPD rate is between 10–15%, compared to lower-income countries like Pakistan and Zimbabwe, which have an estimated PPD rate of 18.6%.34, 35
Because the rate of PPD for teen mothers is estimated to be twice as high as the average US rate of 10–20%, at least 30,000 adolescent girls suffer from PPD every year in the United States.36, 37, 38 Within the US, rates are highest in the Deep South and lower in the Northeast and the West.39 There is also a racial disparity in the US—black and Hispanic women are more likely to experience symptoms of PPD than white women but less likely to seek treatment for maternal depression.40, 41
Contributing Factors
Social Rejection and Exclusion
Social stigma is the disapproval of a group of people with a distinguishing characteristic.42 Teenage mothers are often stigmatized, which causes young pregnant women and mothers to struggle with mental and physical health issues. One study reported that 39.1% of teen moms in a Texan hospital felt stigmatized because of their pregnancy when asked whether they were “worried about what others thought of [them] when [they were] pregnant.43
Some of the stigma associated with adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. stems from the belief that young women are often irresponsible for becoming pregnant while in high school and/or unmarried. As a result of these negative beliefs, young mothers can be ostracized from society and receive low emotional support in their communities, with community members even glaring or verbally rebuking teen moms in public.44 Social stigma can also cause rejection of teen moms in schools: one Michigan school banned pregnant teens from appearing in their school’s yearbook for fear of promoting teenage motherhood, and a high school in Louisiana banned teen moms from their campus altogether.45
Education and work allow adolescent mothers to build social support outside of the home, but teen moms struggle to become educated and succeed in their careers.46 Teen moms are only 40% likely to finish high school and 2% likely to finish college before age 30.47 Due to the education disparity between teen moms and their peers, they are less likely to go into full-time work.48 Because adolescent mothers suffer in the education and career fields, they are excluded from important social communities—consequently putting them at risk for developing PPD. Lower levels of education (less than 12 years) increased postpartum depression from 15.66% to 19.84%, and low amounts of social support increased PPD from 15.15% to 32.03%.49
American media outlets reinforce negative stereotypes regarding teen pregnancy and motherhood, which causes young mothers to doubt themselves. In 2013, NPR reported on a series of ads circulating in New York City that discouraged teen pregnancy.50 In the ads, pictures of babies said things like, “I'm twice as likely not to graduate high school because you had me as a teen,” and, “honestly, Mom, chances are he won't stay with you.”51 The message of this ad campaign perpetuates the stereotype that teenage mothers will end up being abandoned by their child’s father and that young age prevents moms from successfully raising their child(ren). In addition, young mothers report frequent criticism about their parenting skills and abilities, which lowers their self-confidence in their parenting style.52 Adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. feel insecure and doubtful of their parenting ability because of social stigma, and low self-esteem increases the rate of PPD by 14.09% among mothers.53 Social stigma and the low self-esteem it causes contribute to increased levels of postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 in adolescent mothers.
Substance Abuse
Substance abuseSubstance abuse occurs when a person consumes too much alcohol, drugs, or other illegal/legal substances or misuses those substances. Addiction and substance abuse are not the same conditions, as people who abuse substances can stop their behavior(s).4 (including alcoholism and drug addiction) affects a woman’s pre and post-natal experience and increases a mother’s likelihood of experiencing postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2. Between 19.7%–46% of women with a history of substance abuse develop postpartum depression, compared to the overall average of 10–20% of women.54, 55 Adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. are at a high risk for abusing substances, which contributes to their postpartum struggles. Teen moms are more likely to have abused substances in the pre- and post-pregnancy periods than their non-pregnant peers.56 This increase could be because 60% of teen moms drop out of school, and high school dropouts are more likely to smoke, use illegal drugs, and drink alcohol than teens still in high school.57, 58 Specifically, dropouts are more than twice as likely to smoke cigarettes and are 12% more likely to smoke marijuana.59 Adolescent mothers are also more at risk for substance abuse than adult mothers—young women are twice as likely to abuse illegal drugs than older women (older than 26).60
Substance abuseSubstance abuse occurs when a person consumes too much alcohol, drugs, or other illegal/legal substances or misuses those substances. Addiction and substance abuse are not the same conditions, as people who abuse substances can stop their behavior(s).4 causes postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 because it directly impairs a mother’s physical, emotional, and mental health. Alcohol affects chemicals in the brain and impairs the body's functions.61 Excessive drinking causes chemical intoxicants to be released, which increases the frequency of negative emotions.62 Because pregnancy can increase stress levels, pregnant women may start or continue to abuse binge drinking as a coping mechanism.63 Drinking during pregnancy can also lead to a child developing Fetal Alcohol Spectrum Disorder (FASD), which impairs cognitive development. FASD increases stress, anxiety, and depression in the parents; therefore, abusing substances during pregnancy increases the mother’s risk of developing postpartum depression.64, 65 A study found that substance abuse increased PPD rates in adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. from 24% to 44%, evidence of substance abuse’s effect on postpartum depression.66
Paternal Involvement
Co-Parenting
Mothers experience less postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 when they have a stable family life with an involved co-parent. However, teen mothers often lack a stable co-parenting relationship, as 8 in 10 teen fathers do not marry their child’s mother, and most teen relationships involving a child end within the first year of their child’s birth.67 As a result, teenage mothers are less likely to have a stable partner. Because mothers who reported partnership satisfaction involving intimacy had lower rates of PPD (only 17.11% of satisfied mothers had PPD, compared to 39.96% of unsatisfied mothers), adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. are more likely to develop postpartum depression.68
Photo by Vera Arsic from Pexels
A healthy co-parenting relationship often requires living together with your partner and child(ren). Still, only ¼ of teen fathers live with their child’s mother at the time of birth, depriving the majority of teen moms of a supportive co-parent in the home.69 Researchers observed postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 at lower rates among adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. when they viewed their partners as involved, and absent partners certainly do not qualify as involved parents.70 Because healthy partner relationships lower PPD and many teen fathers are uninvolved with their child’s life, teen moms have a higher risk of developing postpartum depression.
Financial Involvement
Women are 15.9% more likely to develop maternal depression when suffering from financial problems, and an absent father figure can contribute to financial stress.71 Higher education is a way to gain career success, but only around 10% of teen mothers attend a 2- or 4-year college program compared to 32.5% and 43.1% of childless women who obtain an associate’s or bachelor’s degree.72, 73 Those without a college degree have a lower median weekly income than those with college and graduate degrees ($520.00–774.00 and $836.00–1,836.00, respectively).74 Teen moms are less educated than their peers, so they have a lower chance of obtaining financial success.
Because teen fathers are less likely to marry their child’s mother, most teen moms are single mothers. Single mothers are at a financial disadvantage—the average annual income for single mothers in the United States is $23,640.00 compared to $82,000.00 for married parents.75 Teen moms experience increased financial stress due to their fragile economic situation, and this stress can contribute to higher rates of maternal depression.
Consequences
Parenting Stress
Postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 increases physical and mental health struggles in the home and impairs healthy parenting, which increases parenting stress. Researchers measured parental stress (on a scale ranging from 36–180) and found that adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. with PPD reported an average stress score of 80.7 while their non-depressed peers reported 62.4.76
Postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 decreases physical health through its symptoms, such as loss of appetite or fatigue, and worsening health increases parenting stress.77 A study on parental stress concluded that maternal depression contributed to a 0.33% increase in parental distress (among both parents) for every 1% increase in depressive symptoms.78 Essentially, PPD led to elevated rates of stress in parents, adding to the already-large parenting responsibilities. Another study found that overall home functioning decreased by 0.87% for every 1% increase in severity of PPD.
Postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 in mothers correlates to paternal depression in their partners. About half of fathers whose partners were depressed also experienced depressive symptoms, compared to the overall paternal depression estimated rate of 2–25%.79, 80 Fathers with depression are less likely to have positive interactions with their children and more frequently use spanking as a disciplinary method.81 Postpartum depression, and subsequent paternal depression, increase paternal stress and negatively affects the parent-child relationship.
Child Development
Postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 increases the risk to the emotional and cognitive development of children.82 Child development encompasses the physical, emotional, and social well-being of a child until they reach adulthood. Children had a higher likelihood of dealing with stress, emotional instability, economic turmoil, and psychiatric illness if their mother had PPD.83 Similarly, a child’s likelihood of developing mental health problems in the future increased by 5–10% when their mother struggled with mental health issues (the average lifetime risk is already 46.4%).84, 85
Photo by RODNAE Productions from Pexels
Researchers explored the connection between postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 and impaired cognitive development. They found that children whose mothers suffered from PPD were more likely to fail to understand the concept of objects and were more at risk of developing impaired language acquisitions than their peers.86 In regards to behavioral development, children whose mothers suffered from PPD were more likely to have observed behavioral issues and were more likely to show active aggression toward their playmates than children without depressed mothers.87, 88
In addition to PPD’s effect on child development, research associates maternal age with low academic achievement and behavioral issues in children. Higher maternal age increases math and reading achievement in children and reduces behavioral issues.89 Additionally, children of young mothers score lower on cognitive tests and are at a higher risk for poor academic achievement.90 Children with adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. have more academic and behavioral problems because teen moms are less knowledgeable about parenting skills and child development than adult mothers.91 The combination of low maternal age and PPD puts the children of depressed adolescent mothers at high risk for struggling with development.
Infanticide and Suicide
Severe cases of postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2, especially those classified as postpartum psychosisPostpartum psychosis (PPP) is an escalation of postpartum depression and a serious mental illness that can cause women to have delusions, hallucinations, paranoia, rapid mood swings, etc., associated with their role as mothers.3, cause mothers to feel violent urges towards themselves and their child(ren) and increases the risk of mothers committing suicide and infanticideThe act of killing a child before they reach the age of 1. The child's parent commits most infanticide cases.. Forty-one percent of mothers with PPD have thoughts about harming their child.92 Although most depressed moms do not act on these feelings, some who suffer from postpartum psychosis do. Postpartum psychosis is considered a medical emergency because of the risk to both mother and child. Out of mothers who suffer from delusions due to PPP, 36% believe their child is the devil, and 21.5% believe their child is not theirs.93 Four percent of mothers suffering from postpartum psychosis commit infanticideThe act of killing a child before they reach the age of 1. The child's parent commits most infanticide cases..94
For reference, the overall infanticide rate in the US is 7.2 (per 100,000 people), thus 0.0072% of all mothers commit infanticide.95 A high-risk factor for infanticide is adolescence. Mothers younger than 15 committed infanticide at a rate of 28.1 (per 100,000 births), mothers aged 15–16 committed infanticide at a rate of 22.0, and mothers aged 17–19 committed infanticide at a rate of 18.8.96 In comparison, mothers ranging in age from 20 to 24 committed infanticide at a much lower rate of 10.7, and mothers 25 years and older committed infanticide at only 4.1.97 The risk of infanticide increases as maternal age lowers, and the jump in infanticide risk between mothers aged 19 and 20 clarifies that adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. commit infanticide at higher rates than adult mothers.
Suicide is the leading cause of death among mothers within the 1st year postpartum.98 Postpartum psychosisPostpartum psychosis (PPP) is an escalation of postpartum depression and a serious mental illness that can cause women to have delusions, hallucinations, paranoia, rapid mood swings, etc., associated with their role as mothers.3 causes a significant risk to mothers, as 5% of mothers who suffer from PPP commit suicide.99 Maternal suicide often occurs when experiencing a psychotic episode because psychosis causes mothers to experience breaks from reality.100 The elevated risk of suicide and infanticideThe act of killing a child before they reach the age of 1. The child's parent commits most infanticide cases. is why postpartum psychosis is considered dangerous; thus, mothers suffering from PPP are encouraged to seek help immediately.101 Maternal suicide is also affected by age. In 2017, 9.5% of mothers under age 19 were suicidal, compared to 1.9% of mothers aged 19–26 and 0.3% of mothers over 26.102 Therefore, adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. suffering from severe postpartum illness are at a higher risk of committing suicide.
Practices
Breastfeeding
The American Academy of Pediatrics (AAP) recommends exclusive breastfeeding until a baby is 6 months old to provide mother and child with health benefits.103 Exclusive breastfeeding requires mothers to feed their baby with breast milk and no other food or drink (even water).104 Breastfeeding provides many benefits for the mother and child, but it is often hard for mothers to exclusively breastfeed their baby. Contrary to the AAP recommendation, only 19.3% of adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. exclusively breastfed their child at 3 months postpartum. Adolescent mothers breastfeed at lower levels than adult mothers—36.4% of mothers in their 20s and 45.0% of mothers older than 30 were exclusively breastfeeding at 3 months postpartum.105 Mothers cite different reasons for abandoning breastfeeding, such as lactation issues, concerns about the baby’s or mother’s health, unsupportive career situations, or lack of family support.106 Unsuccessful breastfeeding, or the abandonment of breastfeeding, can occur when lactation fails, the infant cannot latch, or a mother lacks confidence in the practice.107
New evidence from 2018 suggests that breastfeeding can reduce the risk of postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 and help mitigate PPD symptoms. Researchers conducted a test on mothers (with an average age of 19)—postpartum depressive scores among mothers who were breastfeeding 6 months after the birth of their child were 12.45% lower than the scores of mothers who were not breastfeeding 6 months postpartum.108 Following the AAP recommendation to exclusively breastfeed for 6 months after giving birth can decrease PPD in new mothers because breastfeeding can improve mood and stress symptoms of PPD.109, 110 However, breastfeeding’s effect on PPD is different among women who had good or bad experiences with breastfeeding. A mother’s breastfeeding experience can become negative if she experiences pain, discomfort, or failure while attempting to breastfeed.111 A study found that early negative experiences with breastfeeding increased the risk of postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 at 2 months postpartum.112 Women who reported severe pain while breastfeeding were twice as likely as their counterparts to experience depressive symptoms—because women with breastfeeding pain or difficulties are more likely to suffer from PPD, they should seek screening for maternal depression.113 Because depressive symptoms are associated with negative breastfeeding experiences, breastfeeding should only be encouraged if a mother has a positive experience.
Interpersonal Psychotherapy
Interpersonal psychotherapy (IPT) is a practice that effectively treats postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2 in adolescents. Interpersonal psychotherapy is a specific branch of therapy that focuses on a clients’ current needs and interactions rather than their past trauma.114 IPT defines depression as a medical illness that can be treated and focuses on eliminating self-blame. The three phases of IPT happen over a 12 to 16-week period; these phases are 1) identifying a diagnosis, 2) using specific strategies to deal with one of four possible problem areas, and 3) helping the patient become more self-reliant in dealing with their mental health.115 The 4 problem areas IPT addresses are grief/complicated bereavement, role dispute, role transition, and interpersonal deficits.116 IPT was originally developed for research intervention but is growing in popularity among clinical therapists. The International Society for Interpersonal Psychotherapy (ISIPT) is working on training clinical therapists to practice IPT.117
A study tested preventive methods to combat PPD in adolescents and found that adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child. treated with IPT had a PPD rate of 11.1% at 6 months postpartum, while adolescents who underwent a control treatment had a PPD rate of 25.0%.118 When researchers treated depressed pregnant girls with IPT, they had lower levels of depressive symptoms during motherhood, according to the EPDS (Edinburgh Postnatal Depression Scale). The EPDS classifies depression as scoring at least a 10, and study participants went from an average score of 15.4 to a 9.1, crossing the threshold from depressed to non-depressed.119
While IPT significantly lowered depressive symptoms in adolescent mothersA woman who gives birth when they are the age of 19 or younger and chooses to parent their child., this treatment has not been tested to prevent postpartum depressionPostpartum depression (PPD), also referred to as maternal depression, is a type of depression a mother may experience following childbirth and is generally attributed to stressful life events, low social support, pregnancy complications,1 and negative birth experiences.2, and not all adolescent mothers have access to IPT. Interpersonal psychotherapy does not prevent PPD because medical professionals must first diagnose adolescent mothers with postpartum depression to use IPT. Additionally, IPT can cost anywhere between $75.00–$175.00 per session (depending on the region), and not all adolescent mothers can afford to pay these costs.120 To make IPT a more effective treatment for PPD in adolescent mothers, IPT needs to be provided early in motherhood and at affordable prices.
Preferred Citation: May, Susan. “Postpartum Depression among Adolescent Mothers in the United States.” Ballard Brief. May 2022. www.ballardbrief.byu.edu.
Viewpoints published by Ballard Brief are not necessarily endorsed by BYU or The Church of Jesus Christ of Latter-day Saints